Cardiovascular system Varicose veins
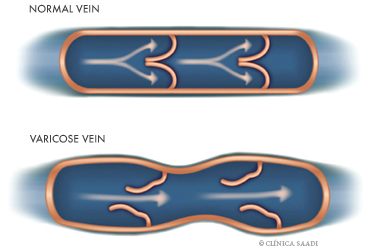
The varicose veins are dilated, tortuous, and elongated veins under the skin, which constitute one of the commonest cardiovascular conditions among all of them. They affect about 15% of the general population.
The varicose veins can be divided in proper varicose veins (according to the definition above) and telangiectasias or varicose microveins, which are small reddened little vessels.
Telangiectasias, varicose microveins, or vascular spiders are intradermal capillaries or venules that dilate and occur mostly in the thigh. The cause of their appearance is not very known, but there seems to be an involved hormonal factor, mainly estrogen, and they are commoner in females. They can become symptomatic in menstruation and increase in pregnancy and with the use of oral contraceptives.
Both variations occur more in females and increase with age. Varicose veins are bilateral in the great majority of cases (75%).
Most varicose veins result from a genetic or familiar predisposition that causes elasticity loss in the vein walls and incompetence of the venous valves. These are called as primary or essential varicose veins and are more frequent.
There are several risk factors in the development of varicose veins, with age being one of the most significant. Varicose veins are extremely rare in children and progressively increase with aging, reaching more than 70% of the people older than 70 years old. This suggests that, at least in part, there can be a degenerative component of the vein itself as the time passes.
Females are more predisposed than males, at a ratio of up to 4:1. There is probably influence of hormonal factors and gestations.
The racial factor has been frequently discussed, and there is a very low prevalence in African Black people and in Arab, Hindu, and Asiatic populations. On the other hand, the prevalence is extremely high in Western White people.
Obesity can be also a triggering factor for varicose veins by the greater abdominal compression over the lower vena cava.
The predominant posture during work as being a cause for varicose veins is debatable, but a permanence for long periods standing up or at sit-down position can worsen a preexisting disease, as well as a sedentary lifestyle, as physical exercise (mainly walk) contributes for their prevention.
There are still some factors that are still not well-documented, such as diet and use of hormones, which can play a significant role in the varicose veins and their clinical manifestations.
Referring to the symptoms, the main complaints of patients with varicose veins are, besides the unpleasable esthetic appearance, also pain, tiredness, and weight on legs, mainly by the end of the day, with these symptoms improving when the legs are raised. The association between symptoms and varicose veins of lower limbs has hard characterization. The pain, the feeling of weight and tiredness on the legs, cramps, and edema are related to larger varicose veins, while only the feeling of weight is more related to telangiectasias.
The diagnosis is made in almost all cases only with a careful clinical history and a well-conducted physical exam. The permeability of the deep venous system, the valvar incompetence, and the reflow can be evaluated with an echodoppler in selected cases.
The complications that can occur are: superficial thrombophlebitis (inflammation and thrombosis of the diseased vein), causing much pain and transient incapacity for work, but very rarely pulmonary embolism; ocher dermatitis with alteration of skin color (darkening); and leg bleeding and ulceration, with these three last ones occurring in chronic cases and without treatment.
Treatment and Procedures
Since the time when Hippocrates cauterized varicose veins with hot iron, the treatment of this disease has evolved a lot and, currently, most patients with varicose veins can be comfortably treated, with excellent esthetic and functional results. The treatment must be individualized and the judgment must be judicious, as there are no magic formulas applicable to all cases. There is frequently need for associating more than one mode of treatment in a same patient.
Essential Varicose Veins
A) Clinical Treatment: Many patients with varicose veins can be clinically treated. The patient must be oriented to avoid prolonged periods standing up or sitting down, obesity, and sedentary lifestyle. Other measures to be prescribed are:
– elastic socks (medium or high compression) must be put in the morning, before leaving the bed, and must be only removed at night;
– raise the legs for 10-15 minutes, 3 times daily;
– walk regularly, for at least 20 to 30 minutes daily, in order to exercise the musculovenous pump in the calf;
– prevent trauma to the varicose veins.
These measures are efficient to alleviate the symptoms, but do not interfere with the esthetic stress of the varicose veins.
B) Surgical Treatment: The varicose veins can be treated by surgery, with excellent esthetic and functional result. The best candidates for surgery are active and non-obese individuals. The indications for surgical treatment are hemorrhage, superficial thrombophlebitis, ulceration, and persistent pain, besides the esthetic reasons.
There is a current trend to preserve the major saphenous vein and to perform more conservative procedures, with microincisions and crochet needles, with no need for stitches in the great majority of times, causing the procedure to be simpler and to result in a better esthetic result.
Telangiectasias or Varicose Microveins
A) Sclerotherapy: This consists in the injection of a sclerosing liquid inside the vein, aiming to injure the endothelium (internal vessel coating), so causing a thrombosis that closes the vessel and is absorbed as the time passes.
B) Laser (Photoderm): More recently, laser and pulsed light (Photoderm) are being used for treating telangiectasias and other benign vascular lesions. This non-invasive treatment is performed by emitting high-intensity light pulses. Such light passes through the skin (protected by a chilled gel) and reaches the vessel, so increasing the blood temperature inside it and injuring the endothelium by a mechanism called as photothermolysis. Consequently, there is the closure of such vessels, with later absorption and clearing. The procedure can be also used in face and neck telangiectasias and hemangiomas.
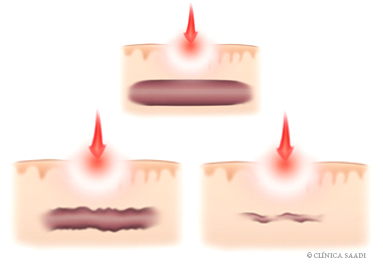
THE VARICOSE MICROVEINS ARE SMALL REDDENED AND DILATED VESSELS VERY FREQUENT IN THE FEMALE POPULATION. MORE RECENTLY, LASER OR PHOTODERM ARE BEING USED TO TREAT THIS DISEASE, BY NON-INVASIVELY EMITTING LIGHT PULSES THAT CLOSE SUCH VESSELS, WITH LATER ABSORPTION AND CLEARING.

